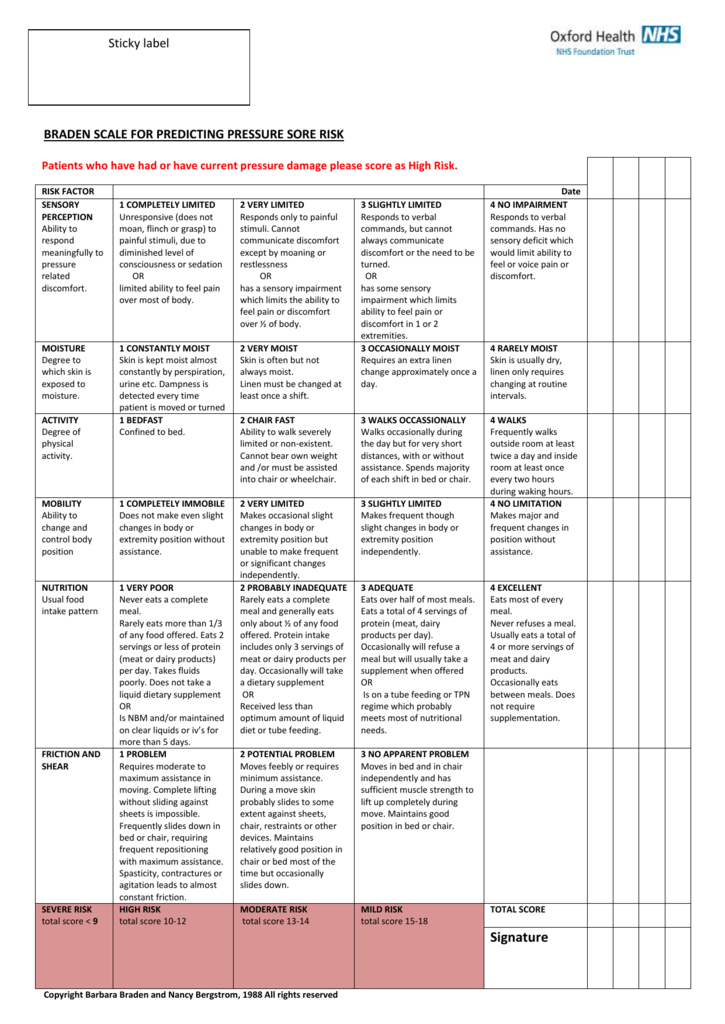
 The Braden Scale for Predicting Pressure Sore Risk is a widely used tool in healthcare settings to assess the risk of developing pressure ulcers or bedsores in patients. Developed by Barbara Braden and Nancy Bergstrom in 1987, this scale helps healthcare professionals identify patients who are at high risk of developing pressure ulcers and implement appropriate preventive measures.
The Braden Scale for Predicting Pressure Sore Risk is a widely used tool in healthcare settings to assess the risk of developing pressure ulcers or bedsores in patients. Developed by Barbara Braden and Nancy Bergstrom in 1987, this scale helps healthcare professionals identify patients who are at high risk of developing pressure ulcers and implement appropriate preventive measures.
Understanding the Braden Scale
The Braden Scale consists of six subscales, each assessing a different aspect of the patient’s risk factors for pressure ulcers. These subscales are:
- Sensory perception
- Moisture
- Activity
- Mobility
- Nutrition
- Friciton and shear
Each subscale is scored from 1 to 4, with a lower score indicating higher risk. The scores from all subscales are then added up, resulting in a total risk score between 6 and 23. The lower the total score, the higher the risk of developing pressure ulcers.
Importance of Pressure Sore Risk Assessment
 Pressure ulcers, also known as bedsores, are a prevalent healthcare issue that can lead to serious complications in patients. They occur when prolonged pressure restricts blood flow to the skin and underlying tissues, resulting in tissue damage and the formation of ulcers. Individuals who are immobile or have limited mobility, such as elderly or critically ill patients, are particularly susceptible to developing pressure ulcers.
Pressure ulcers, also known as bedsores, are a prevalent healthcare issue that can lead to serious complications in patients. They occur when prolonged pressure restricts blood flow to the skin and underlying tissues, resulting in tissue damage and the formation of ulcers. Individuals who are immobile or have limited mobility, such as elderly or critically ill patients, are particularly susceptible to developing pressure ulcers.
By using the Braden Scale, healthcare providers can accurately identify patients at high risk of developing pressure ulcers. This allows for early intervention and the implementation of preventive measures, such as regular repositioning, skin care, specialized support surfaces, and nutritional interventions. Early identification and prevention of pressure ulcers can significantly improve patient outcomes, reduce healthcare costs, and enhance the overall quality of patient care.
The Braden Scale in Practice
 The Braden Scale is widely used in various healthcare settings, including hospitals, long-term care facilities, and home healthcare. It is typically administered upon admission and then regularly reassessed to monitor changes in the patient’s risk status. Healthcare professionals, such as nurses and wound care specialists, are trained to administer the scale and interpret the results accurately.
The Braden Scale is widely used in various healthcare settings, including hospitals, long-term care facilities, and home healthcare. It is typically administered upon admission and then regularly reassessed to monitor changes in the patient’s risk status. Healthcare professionals, such as nurses and wound care specialists, are trained to administer the scale and interpret the results accurately.
The Braden Scale is an integral part of pressure ulcer prevention protocols and is often incorporated into electronic health records to ensure consistent assessment and documentation. It serves as a communication tool among healthcare providers, enabling them to identify patients who require specialized interventions and allocate resources accordingly.
Conclusion
 The Braden Scale for Predicting Pressure Sore Risk is a valuable tool in the prevention and management of pressure ulcers. By assessing various risk factors, it helps healthcare professionals identify patients at high risk and implement targeted preventive measures. This scale plays a critical role in improving patient outcomes, reducing healthcare costs, and enhancing the overall quality of care provided. It is important for healthcare professionals to remain vigilant and routinely use the Braden Scale to identify patients who may require additional interventions to prevent pressure ulcers.
The Braden Scale for Predicting Pressure Sore Risk is a valuable tool in the prevention and management of pressure ulcers. By assessing various risk factors, it helps healthcare professionals identify patients at high risk and implement targeted preventive measures. This scale plays a critical role in improving patient outcomes, reducing healthcare costs, and enhancing the overall quality of care provided. It is important for healthcare professionals to remain vigilant and routinely use the Braden Scale to identify patients who may require additional interventions to prevent pressure ulcers.
References: